Trusted for 24+ Years
Perimenopause & Menopause Solutions

Dr. Lisa Lawless, CEO of Holistic Wisdom
Clinical Psychotherapist: Relationship & Sexual Health Expert

Mastering the Challenges
Women, trans men, nonbinary, and genderqueer people can all go through perimenopause and menopause. Menopause begins naturally when a the ovaries start making less estrogen and progesterone, the hormones that regulate the menstrual cycle. This gradual hormonal change gets underway as early as the late 30's but typically occurs between 45-55 years of age.
The transitional period is called perimenopause and can last from two to ten years, starting with the first year after your final period. The perimenopause phase is a natural part of aging and is a sign of the beginning of the end of the reproductive years. During this period, many experience uncomfortable symptoms that may feel overwhelming or challenging to manage.
For some, this transitional period can last for years, whereas others transition to menopause within just a few months. What seems to matter most in the severity of symptoms is the other burdens one may have placed on their bodies over the years.
Chronic stress, lack of exercise, and poor nutrition are three significant players as they considerably affect the body's ability to detoxify and maintain homeostasis. Other lifestyle choices such as consuming excessive amounts of alcohol and smoking are also compounding factors. With this said, healthy lifestyle modifications will make a significant difference in lessening the uncomfortable symptoms associated with perimenopause.
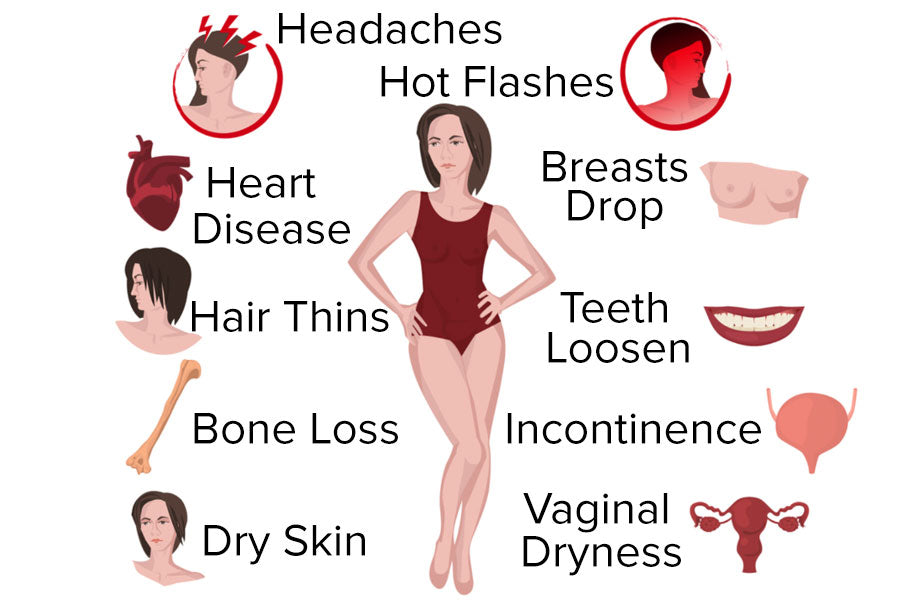
This article offers some information and tips on how you can master the symptoms of this natural transitional phase of a one's life. Below are some telltale signs of perimenopause:

Menstrual Irregularity
Irregular menstrual cycles are characteristic of perimenopause. When hormones fluctuate and ovulation becomes more erratic, you may experience much heavier or lighter menstrual flow, and menstruation may last a longer or shorter times.
You may skip some periods. However, if any of the following occurs, you should see your doctor as these may be symptoms of a serious gynecological problem:
- Extremely heavy bleeding where you are replacing your tampons or pads every hour.
- Bleeding that lasts longer than 8 days.
- Bleeding occurs between periods.
- Regular occurrence of periods less than 21 days apart.
Changes in Mood
Some can experience mood swings, irritability, or depression during perimenopause, but there is debate about what causes these mood changes. Some researchers believe brain changes that cause depression, irritability, and anxiety are brought about by the change in estrogen levels. Others believe these mood fluctuations are influenced by other symptoms of perimenopause, including hot flashes, night sweats, fatigue, and troubled sleep and not by changes in your hormones.
Still, some speculate that it is a combination of both changing hormone levels and perimenopause symptoms. The good news is you don't have to accept mood changes as a "normal" part of perimenopause; with proper treatment and holistic health support, you can feel more like yourself again.
Perimenopause & Menopause Can Cause Anxiety and Panic Attacks
It is not uncommon to experience anxiety and panic attacks during perimenopause and menopause. It is prevalent for those with pre-existing anxiety and may evolve into a panic disorder. Women aged 50–79 years are the age group where the most panic attacks occur. Panic attack symptoms can be physical and psychological, including symptoms like:
- Heart palpitations
- Chest pains
- Sweating
- Shaking
- Nausea
- Dizziness
- Sense of doom
- Numbness
- Anxiety
- Chills
The most common treatments for menopause-related anxiety include low-dose hormone replacement therapy (HRT). In addition, antidepressants, anti-anxiety medication, psychotherapy, a healthy nutrition-focused diet, or supplements for improved mood. Avoid eating sugar as it can cause increased anxiety.
Cognitive behavior therapy (CBT) is effective as a treatment for menopause. CBT is primarily used to treat depression and anxiety disorders and helps people learn how to identify and change negative thought patterns that affect them.
Herbal supplements that can help calm the body are holy basil (tulsi), chamomile, hops, passion flower, ashwagandha, lemon balm, kava, and others. Make sure to check with your physician or pharmacist regarding any herbs you take, as they too are a form of drugs and may affect other health conditions or interfere with medications you may be taking.
Anxiety & Related Cardiovascular Symptoms
Hormonal fluctuations during menopause may negatively affect the cardiovascular system. Perimenopause and menopause may cause heart palpitations. First, it is essential to rule out heart conditions by working with your physician, especially a cardiologist, because post-menopausal women are more likely to develop heart disease and arrhythmia than pre-menopausal women.
It is typical for cardiac arrhythmias such as an abnormally fast heart rate, leading to shortness of breath, chest pain, and severe anxiety. Women who experience fast heart rates (tachycardia) may be prescribed medications known as beta-blockers, which can regulate the heart's rate and rhythm and ease other physical manifestations of anxiety, including sweating, shaking, hyperventilation, and apprehension.
How To Redirect Your Brain When You Feel Panic & Anxiety
- Stay focused on the present and ask yourself what you can do when experiencing worry. If you are safe and alright, make a time where you will check in with yourself to revisit your concerns when you are in a better emotional place.
- Relabel your feelings when you feel panic. Often, it can feel like you are dying or having a heart attack. Remind yourself that this is a panic attack and tell yourself that it is temporary and that you do not need to do anything right now. Your body is activating its flight or flight response to keep you alive, and it is essential to refocus your mind to understand that you are safe and alright. If you can, crying is an excellent way to release these challenging feelings as it activates the vagus nerve and parasympathetic system. It can relieve stress and decrease cortisol levels in the body.
- Fact check your thoughts by challenging how realistic they are, so instead of focusing on feeling anxious, say things to yourself that assure yourself that you are alright, prepared and that things will go well. Rethinking your fears trains your brain to deal with your anxious thoughts.
- Breathe in and out slowly by evenly inhaling and exhaling. This will help slow down and refocus your mind.
- Follow the 3-3-3 rule by naming three things you see and hear. Then move three parts of your body (i.e., touch a finger to your nose, lift a leg and pat your head three times). By doing this, you are activating a different part of your brain, which will help manage your emotions.
- Do a task such as get up and put something away, get a glass of water or action as it will interrupt your anxious train of thoughts and help you feel more in control.
- Stand up straight and pull your shoulders back with your feet apart. When we are stressed, we hunch, and it makes us feel as though we are cowering to protect ourselves. When we stand up straight, we can feel more in control.
- Process your feelings with a trusted friend or partner and ask them how realistic you are about your worries. You can also write out your fears to better see what you are worrying about.
- Watch something funny, especially short clips that quickly redirect your attention. Laughing allows us to release tension and lowers anxiety.
- Exercise to release pent-up energy and channel it into a physical activity that makes you sweat. This helps the body boost your endorphins which make you feel good.
- Use paired muscle relaxation to relieve tension. While taking a deep breath in, tense the muscles of your entire body. Notice how that tension feels. When you breathe out, let go of all that tension and notice the changes you feel in your body. You can also try tensing specific muscle groups such as legs, arms, etc.
- Sit or take a walk outside in nature or simply watch the clouds pass. Nature is known to improve mood, reduce anxiety, lower blood pressure and stress hormone levels, reduce nervous system arousal, enhance immune system function, and increase self-esteem.
- Redirect your stress by giving your body something to taste. For example, drinking relaxing herbal tea, chewing gum, or sucking on sugar-free candy can help you to relax.
- Using scents to lift your mood can be helpful. Using essential oils in diffusing oils, wax melts, or scented candles can be beneficial. Even putting on your favorite scent can help you to relax.
- Massage, acupuncture, relaxing baths, and other forms of physical soothing can allow you to destress.
- Listening to your favorite music, using a sound machine, and repeating positive affirmations can help reduce stress.
Reset The Vagus Nerve During Anxiety: Polyvagal Theory Exercises
Resetting the vagus nerve, which interfaces between the central nervous system and consists of the brain and the spinal cord, can be helpful as it can release anxiety that is physiologically happening in the body. You can do this through polyvagal exercises. Examples of this:
- Hold your face under cold water for 15 to 30 seconds or put a ziplock bag over your face with ice water in it. This will trigger your brain to think it is diving underwater, slowing your heart rate.
- Using vocal sound can help stimulate the vagus nerve as it is located near the vocal cords. To do this, yoga practitioners recommend the "om" chant or other mantras, but simply humming any song can have the same effect.
- Lie on your back, interlace your fingers, and place them behind your head at the base of the skull. Keeping your head straight, move your eyes to the right, sigh, swallow or yawn and then move your eyes to the left and do the same; you may blink during the exercise. Do this for about five minutes or until you feel calmer.
Paresthesia
Paresthesia is an abnormal sensation of the skin (tingling, pricking, chilling, burning, numbness, itching) that can occur due to a sharp decline in estrogen. It can cause distress in women who experience it. Vitamins and minerals such as biotin, magnesium, vitamin C, and omega-3 fatty acids may assist with skin issues during menopause.
Sleep Disturbances
Those who have slept soundly their entire lives may find that fluctuating hormone levels wreak havoc with their sleep cycle. Hot flashes or night sweats often cause difficulties falling asleep or staying asleep along with hormonal fluctuations.
Hot Flashes
It is essential to stay hydrated because hot flashes and night sweats cause profuse sweating; they can also cause electrolyte loss through perspiration, dehydration, and insomnia.
Itchy Skin
Itchy skin is something that is often overlooked when it comes to menopause. However, some women may experience itchy skin (pruritus) all over their bodies, including itchy sensations inside the ears. An itch inside ears, which can be intense, is often misdiagnosed by physicians as eczema or other ailments when in reality, it is just part of perimenopause or menopause. However, keep in mind that hormone levels that change during menopause can lead to some women developing eczema.
Vaginal Changes and Bladder Problems
Estrogen plays a crucial role in maintaining the function of the vagina and surrounding tissues, uterus, urinary bladder, and urethra (the organ through which urine is passed from the bladder). As these tissues weaken, they can lead to the involuntary leakage of urine, infection, or painful urination. The vaginal tissues also become less lubricated, which can cause uncomfortable or even painful sexual intercourse and more frequent urinary tract infections.
See our Kegel Exercise Guide and Kegel Weights Guide to prevent or help with urinary incontinence.
Decreasing Fertility
As hormones fluctuate and ovulation becomes irregular, your ability to conceive decreases. As long as you have periods, pregnancy is a possibility. If you do not want to conceive, it is recommended that you use birth control until you have reached menopause and have not had a period for 12 months.
Bone Loss
As estrogen levels decline, you naturally begin to lose bone more quickly than you replace it, thus increasing your risk of osteoporosis. The best things that you can do for your bones are below:
- Get enough calcium and vitamin D3 and eat a well-balanced diet. Plant-based is ideal as fruits and vegetables are nutrient-dense and high in fiber, which helps regulate hormones.
- Avoid smoking and limit alcohol. See our article on Wine, Chocolate & Health Guide for more information.
- Engage in regular exercise like walking, yoga, cycling, etc. If you have osteoporosis, avoid high-impact exercises or activities in which a fall is likely. Also, avoid activities that put weight or heavy stress on the spine to prevent fractures.


Change in Cholesterol Levels
Declining estrogen levels may also negatively affect your blood cholesterol levels. This could include an increase in low-density lipoprotein (LDL) cholesterol (the "bad" cholesterol), which contributes to an increased risk of heart disease. At the same time, high-density lipoprotein (HDL) cholesterol (the "good" cholesterol) decreases in many as they age, which also increases the risk of heart disease.
Low Libido
You may find your sexual desire and arousal change during perimenopause. Hormonal imbalance is the most common cause of low sex drive during this phase of life. The hormone progesterone plays a significant role in libido. As progesterone levels drop, it can affect your sexual desires and state of arousal.
However, keep in mind that libido may not decline with the onset of menopause because estrogen declines more than testosterone. Thus, some theorize that a lower sex drive should not be an issue because of estrogen reduction. The decline in testosterone is related to age, not menopause, and begins years before perimenopause.
Declining estrogen levels also affect testosterone, which plays a role in sexual response and orgasm. Fatigue caused by hormonal imbalance and poor nutrition can also affect your interest in sex.
Sexual Aids For Perimenopause & Menopause
The symptoms of perimenopause result from changing hormone levels that some begin noticing long before menopause takes place. Using sexual aids such as sex toys, lubricants, Kegel exercisers, and even dilators can be helpful.
Vibrators
Vibrators help increase blood flow to the genital area and thus bring helpful circulation, which can aid in increasing the sex drive (libido), increase lubrication, and assist in achieving orgasms. See our guide on How To Choose A Vibrator.
Lubricants
Lubricants help reduce friction during vaginal penetration and be used as vaginal moisturizers to help with vaginal dryness that can cause painful sex during perimenopause and menopause. See our helpful Lubricant Guide for helpful tips.
Dilators
Sometimes during perimenopause or menopause, vaginal tissue can become dry, making sex painful. With sexual inactivity, the vaginal walls may also become tight, making sexual penetration more difficult. Using dilators to stretch can be helpful.
Kegel Weights
Kegel weights and exercisers can help make the vagina feel tighter and more snug which can improve one's sex life. However, the most common reason is that many struggle with urinary incontinence, causing embarrassing leaks, especially when laughing, sneezing, coughing. This can be exacerbated by childbirth recovery, weak pelvic floor muscles, and pelvic organ prolapse. Doing Kegel exercises with or without Kegel weights for just 10-15 minutes a day can make a big difference.
Lifestyle Modifications
Exercise
Recommendations are three to five days a week of exercise, including resistance or weight training with weights, bands, machines, and cardiovascular activity such as brisk walking, cycling, swimming, or aerobic type classes. Also, stretching should be done most days of the week to maintain range of motion. Yoga, pilates, and tai chi classes can be a valuable activity of this age group.
Why Is Exercise So Important?
- Engage in regular exercise as it increases the cardiorespiratory functioning and reduces metabolic risks associated with declining estrogen.
- Exercise increases HDL, reduces LDL, triglycerides, and fibrinogen, which lowers the risk of high blood pressure, heart attacks, and strokes.
- Exercise minimizes midlife weight gain. It increases the metabolism to burn off the extra fat gains associated with hormones change. Also, see our Weight Loss Guide.
- Exercise also increases bone mass and can help offset the decrease of bone mineral density and prevent osteoporosis.
- Reduces lower back pain associated with perimenopause and menopause. Research has associated low estrogen levels with more severe lumbar disc degeneration and increased lower back pain in menopausal women.
- Exercise reduces stress and improves mood. Exercise releases endorphins in the brain, which stimulates a feeling of well being that can last several hours and help alleviate some depression and mood swings.
- It may reduce hot flashes, and studies have shown that hot flashes are also less common among physically active people who exercise regularly.
Nutrition
As your risk of heart disease and osteoporosis increases at this time, a healthy diet is more important than ever. Choose a low in saturated and trans fats and high-fiber diet that's rich in fruits, vegetables, beans, and whole grains such as steel-cut oats. Add calcium-rich foods or take a calcium supplement if your physician suggests it. Eat things like dark leafy greens, which are a great source of calcium, which is essential for maintaining bone health.
The Controversy Of Phytoestrogens In Soy
Soy products contain important isoflavones, and it has been proven that soy products are associated with fewer hot flashes. We recommend soy products high in isoflavones: green soybeans, soy flour (textured), dry roasted soybeans, tempeh, soybean curd cheese, tofu, tofu yogurt, soymilk.
Soy comes from soybeans and is consumed in various ways, such as eating them steamed (edamame), tempeh (fermented soybeans), and soy flour and milk. Soy has high amounts of phytoestrogens, so there has been controversy around its effects on sexuality. There have even been false claims that they increase estrogen levels and increase breast cancer risks. Let's explore why that is not correct.
Your body knows the difference between estrogen and plant-based phytoestrogens. We know this because of the receptors that are used to process them. There are two estrogen receptors in the body, alpha (A receptor) and beta (B receptor). Unlike actual estrogen, which binds to A receptors, soy phytoestrogens bind to the B receptors. This is critical because each receptor has completely different ways of distributing the estrogen and phytoestrogen hormones.
A medical study done in 2004 shows that because the B receptors distribute phytoestrogens, they have an anti-estrogenic effect, meaning that it inhibits actual estrogen. This means that eating phytoestrogens in soy products will not increase estrogen levels.
Websites scaring people away from eating soy, claiming that it contributes to estrogen-related cancers, are wrong, and many studies support that this is false. This also means that those holistic websites promoting it to increase estrogen in perimenopausal and menopausal women are also incorrect.
So how did this rumor that soy causes an increase in estrogen occur? It was based on a study that tested breast cancer in mice, but it turns out that we metabolize soy isoflavones very differently from rodents. Not only that, it turns out through multiple studies that soy actually reduces our chances of breast cancer if eaten regularly. This was further validated and published in 2009 in the Journal of the American Medical Association. It is also why the American Cancer Society recommends consuming soy.
We highly recommend nutrition based on the books "How Not To Die," By Michael Greger, M.D. FACLM and "Eat To Live" by Joel Fuhrman, M.D.
For more information, see our Nutrition Guide for Good Sex & Health Guide.
Reduce or Eliminate Stimulants
It's best for your overall health to stop smoking altogether and try to reduce or avoid alcohol and caffeine. Smoking increases your risk of developing heart disease and reduces bone strength. Alcohol can also reduce bone strength and has been associated with a higher risk of breast cancer. Experts recommend that those going through perimenopause and menopause drink no more than one serving of alcohol each day. Stimulants such as caffeine can also trigger hot flashes and interrupt natural sleep cycles.
Stress Reduction
Stress creates an imbalance in body, mind, and spirit and aggravates the symptoms of perimenopause. If practiced regularly, stress reduction techniques, such as meditation, yoga, and self-imagery, can promote relaxation and good health and are particularly helpful during this phase. Women tend to take care of everyone else, but don't make time for themselves. Treat yourself to relaxation periods throughout your busy schedule to renew your energy and create a positive attitude.
Foot Massage
A study about how foot massage affects anxiety, fatigue, and sleep in postmenopausal women determined that foot massage applied during menopause can increase the average daily sleep duration and reduce fatigue and anxiety levels in women.
This has important implications for women going through this stage of life, as it suggests that regular foot massages, whether from a partner, massage therapist, or other means such as acupressure, may be able to improve their overall well-being and reduce the negative effects of menopause.
Complementary and Alternative Therapies
Complementary and alternative therapies are medical treatments that are considered nontraditional. They include dietary and herbal supplements, acupuncture, chiropractic and massage therapy, biofeedback, homeopathy, and eating certain foods that are thought to prevent disease or heal.
Alternative treatments are often used alone, while complimentary treatments are alternative treatments used in combination with traditional treatments, such as drug treatments or surgery.
Herbal remedies and supplements that have been shown to help counteract perimenopause symptoms while increasing overall health are listed below. Understand that herbs can be just as powerful as a drug and can interfere with medications, so make sure to review all of the herbs you take with your physician and research them thoroughly to ensure that they will meet your health needs and not cause health problems.
Bayberry (Morella Cerifera)
The fruit of the Bayberry tree can increase blood flow and capillary dilation in the mucus membranes of the vagina. This can increase vaginal lubrication. Bayberry also has beneficial effects on female reproductive muscle organs by increasing muscle tissue tone and circulation.
Black Cohosh (Cimicifuga racemosa, Actea racemosa)
A member of the buttercup family and native to North America. Some clinical research has shown that black cohosh is effective for the relief of hot flashes, night sweats, and vaginal dryness. This herb has been proven to reduce luteinizing hormone secretions. High levels of the luteinizing hormone are responsible for the onset of menopause.
Calcium
Essential for the normal growth and maintenance of bones and teeth. Perimenopause and menopause represent depletion of estrogen, which, in turn, is associated with increased risk of bone loss and heart disease. Should be taken with magnesium for optimal absorption.
Damiana (Turnera diffusa)
Damiana is a small shrub native to Mexico. The leaves are used for medicinal purposes. Damiana is considered a powerful aphrodisiac. It stimulates the sympathetic nerves' function controlling the sexual organs, the urinary system, the digestive organs, and the respiratory organs. The herb strengthens all the functions of the sexual organs and urinary system. This herb is especially effective. It has been shown to have the same effects as the hormone progesterone and regulating estrogen, which can benefit premenopausal and menopausal people.
Evening Primrose (Oenothera biennis)
A biennial herb common in North America Parts The seed oil is a good GLA source, an essential fatty acid. An essential fatty acid is a nutrient that the body can't make but is essential to good health. Evening Primrose Oil has been used for premenstrual syndrome ( PMS ) and mastalgia ( sore breasts ). Studies to date have been conflicting; some show a significant reduction in breast pain, while others fail to confirm this. There are no known contraindications or drug interactions reported.
Flax Seed Oil ( Linum Usitatissimum)
A perennial herb grows to 3 ft. with oily brown seeds, native to Europe and Asia. The seeds and seed oil contain essential fatty acids - palmitic, steric, oleic, linoleic, and linolenic. Flaxseed oil is a good source of essential fatty acids. Flaxseed oil is rich in (GLA) gamma Linolenic acid used by many for PMS and breast tenderness. No reports of toxicity when used at recommended doses.
Gingko Biloba
Many research studies have shown Ginkgo Biloba can assist in improving blood flow. Enhancing blood flow to the genitals heightens sexual sensations. Gingko Biloba significantly increases mental activity and memory. Since sexual desire begins in the brain, this herb can be a powerful sexual aid.
Ginseng (Panax quinquefolius)
The several Ginseng species are native to East Asia and Northern America. Ginseng stimulates neural functions and stimulates and normalizes cerebral and sexual organ blood flow. Ginseng also stimulates nerve growth, blood production, and sperm production. This stimulation will, in turn, give a revitalizing effect, stronger sexual arousal, improved genital function, and increased physical sensation.
Horny Goat Weed (Epidemium)
Epidemium is native to East Asia. The entire plant, except for the root, is used in herbal preparations. This herb stimulates the sexual organs, giving enhanced genital sensations. It can also increase sperm production, which may improve fertility. It further stimulates sexual desire by acting upon the central nervous system. This herb has been used for over 2,000 years as a libido enhancer for both men and women and improves erection in men.
L-arginine With Choline
This combination is recommended daily for promoting better blood flow to the pelvic organs and tissue to assist with low libido.
Maca (Lepidium Meyenii)
Maca is native to Peru and has been passed down as a legendary sex-enhancing root from the Incas. Maca root is known for it's the ability to stimulate sexual desire and drive, increase energy, libido, and sexual function. This Peruvian herb may also help with hot flashes and night sweats.
Magnesium
Helps with calcium absorption, acts as a muscle relaxant, produces a sense of calmness, reduces mood swings and irritability, promotes a peaceful night's sleep, and reduces food cravings.
Natural Progesterone Cream
Natural progesterone creams usually contain extracts from Mexican wild yam, a substance that is believed to be similar to the body's progesterone. Many have found natural progesterone creams to be very effective in treating menopause symptoms. Still, there is no evidence to show that the creams lower the risk of breast and uterine cancer, or are free from side effects as is sometimes claimed.
Peppermint (Mentha Piperita)
Leaves of the peppermint plant stimulate genital secretions, which enhance lubrication. This facilitates the sexual act and protects the sexual organ against injury.
Sage (Salvia Officinalis)
The leaf of the sage plant has been used medicinally for centuries. Sage leaf will assist in improving mental focus energy restoration. Sage is a natural antiperspirant that contains estrogen-like substances to help alleviate "hot flashes" and the adverse reactions to hormonal changes.
Suma (Pfaffia Paniculata)
Suma is native to the Amazon Basin. The indigenous people of the Amazon have been using Suma for centuries as a sexual tonic. Suma root is an adaptogen that normalizes hormone production, increases libido, and calms nerves. An improved hormonal system can, in turn, improve mental and physical sexual function.
Valerian (Valeriana Officinalis)
Sleep disturbances are common during perimenopause caused by hormonal fluctuations. Valerian is an effective herbal supplement that decreases the time it takes to fall asleep, improves sleep quality, and reduces the number of night awakenings, all without any associated daytime drowsiness.
Vitamin B6 (Pyridoxine)
Natural sources of vitamin B6 are whole grains, bananas, potatoes, nuts and seeds, and cauliflower. Vitamin B6 levels can be helpful in those who are deficient and suffering from depression. Pyridoxine, folic acid, and vitamin B6 deficiencies have also been associated with osteoporosis in postmenopausal people. At least ten studies have been done on pyridoxine use for PMS and improved PMS symptoms with pyridoxine supplementation. Vitamin B6 is also associated with a decrease in the incidence of heart disease in women. Vitamin B6 is safe when taken in recommended dosages.
Vitamin C
Best when taken with Bioflavonoids (such as Hesperidin), helps boost the immune system, reduce hot flashes, and aid the adrenal glands.
Vitamin E (d-alpha-tocopherol)
An antioxidant found in high amounts in polyunsaturated vegetable oils, wheat germ, seeds, and nuts. In natural vitamin E, the small d in d-alpha-tocopherol signifies a natural source preferable to synthetic vitamin E signified by the dl in dl-alpha-tocopherol. Mixed tocopherols contain d-alpha, beta, delta, and gamma tocopherols. Mixed tocopherols offer the most significant benefit. Look for natural mixed tocopherols. Vitamin E has been shown to help in reducing hot flashes and vaginal dryness. Vitamin E potentiates (cause a more significant effect) of anticoagulant drugs such as Coumadin or aspirin. If you are on either of these drugs, consult your doctor or naturopath before starting vitamin E.
Traditional Medical Treatments
If you have severe symptoms, you may want to ask your doctor about prescription medicines. Some choices include:
Low-dose hormone replacement therapy (HRT)
Low-dose hormone replacement therapy (HRT), which is also called menopausal hormone therapy (MHT), and sometimes estrogen replacement therapy (ERT), consists of medications containing female hormones to replace the ones the body is no longer making. In 2002, a large clinical trial called the Women's Health Initiative (WHI) reported that hormone therapy posed more health risks than benefits for women in the clinical trial. As the number of health hazards attributed to hormone therapy grew, doctors became less likely to prescribe it. And up to two-thirds of women on the therapy discontinued its use, often without talking to their doctors.
Today, there's plenty of confusion about hormone replacement therapy, which is now commonly called hormone therapy. The truth is that hormone therapy is not the magical cure for aging that it was once believed to be, but it's still the most effective treatment for unpleasant menopausal symptoms for most. If you're facing menopause, learn more about the benefits and the risks of hormone therapy.
Low-Dose Birth Control Pills
Helpful in preventing pregnancy and may also have some health benefits. They can reduce hot flashes and vaginal dryness. Very-low-dose birth control pills can also help regulate your periods if they are heavy or irregular. They may also prevent bone loss and helps protect you from osteoporosis.
Another potential benefit is protection from cancer of the ovary and uterus. The lower dose of estrogen in low-dose birth control is believed to be safer for perimenopausal women. Perimenopausal women who have a history of deep blood clots, breast cancer, or heart disease should not take very-low-dose birth control pills. Women who smoke also should not take them.
Perimenopause & Menopause Empowerment
How do you decide what to do? Carefully review your medical history and re-examine your values and beliefs. You will then be better able to determine your goals and how best to achieve them. For example, some women choose only lifestyle changes, like diet, exercise, and relaxation. Others favor herbal remedies and acupuncture. And still, others prefer to use medication. The choice is up to you.
Whatever you choose, know that the most important things you can do are eat a healthy diet, exercise, reduce stress levels, and get enough sleep. Nurture yourself; you are worth it.





