Trusted for 25+ Years
Perimenopause & Menopause Solutions

Dr. Lisa Lawless, CEO of Holistic Wisdom
Clinical Psychotherapist: Relationship & Sexual Health Expert

Mastering the Challenges
Women, trans men, nonbinary, and genderqueer people can experience this fun life stage too so this article is for everyone that goes through these changes.
So, what’s the deal with menopause? Think of it as your ovaries saying, “We’re clocking out!” They gradually start producing less estrogen and progesterone, the VIPs of your menstrual cycle. This hormone rollercoaster can kick off as early as your late 30s (surprise!) but usually hits its stride somewhere between 45 and 55.
This delightful little transitional period, which can last anywhere from two to ten years (because your body loves a good guessing game), starts before menopause officially begins—basically the year after your last period waves goodbye for good.
Think of perimenopause as puberty’s evil twin. It’s a totally natural part of aging—yes, we’re talking about the beginning of the end of your reproductive years—but that doesn’t mean it’s a walk in the park. No, it’s more like a confusing hike through a swamp filled with mood swings, hot flashes, and the occasional “why am I crying over a commercial again?” moment. Manageable? Sure. Annoying and overwhelming? Oh, absolutely. But don’t worry, you’re not alone in this weird, sweaty chapter of life.
For some of us, the road to menopause is a long, winding journey that feels like it’s taking the scenic route—over several years. For others, it’s more like hopping on a high-speed train and arriving at the destination in just a few months.
But here’s the kicker: how bumpy your ride gets seems to depend a lot on what kind of mileage your body has racked up over the years. Stress, lifestyle habits, and even how many times you’ve ignored your own needs to keep everyone else happy—yep, all that baggage comes along for the trip. Buckle up, because this ride? It’s all yours.
Stress, junk food, skipping your morning jog—these aren’t just bad habits; they’re the toxic trio quietly messing with your body’s ability to keep itself clean and balanced. Toss in happy hour that somehow turns into "whoops, the whole bottle’s gone" and those “just one more” cigarettes, and it’s like your body is throwing a rager without your permission.
But here’s the good news: you don’t have to put up with this chaos. A few smart lifestyle tweaks—like actually eating a vegetable or lacing up your sneakers for a walk—can help turn things around.
And if that’s not cutting it? Enter Hormone Replacement Therapy (HRT), the MVP of perimenopause relief. HRT can be the secret weapon your body needs to calm the storm, giving you a shot at feeling like yourself again. It’s not cheating—it’s self-care. Call your doctor, grab a green smoothie, and tell your hormones who’s boss.
So, here’s the deal: perimenopause is like that one friend who shows up unannounced, stays way longer than they’re welcome, and rearranges your entire house while they’re at it. But fear not, my fellow hormonal warriors—we’re here to decode this messy phase and help you boss your way through it.
First things first, let’s talk about the signs that perimenopause has officially RSVP’d to your life party. Think of these as the calling cards of your new, slightly unhinged houseguest:

Menstrual Irregularity
Irregular menstrual cycles are characteristic of perimenopause. So, one day, you’re wearing white pants with confidence, the next, you’re frantically Googling “why is my period trying to ruin my life?”
As your hormones throw an all-you-can-chaos buffet, your menstrual cycle becomes as predictable as a toddler in a toy store. Here’s what to expect when your body goes rogue—and when to call in the pros:
- Extremely heavy bleeding where you are replacing your tampons or pads every hour.
- Bleeding that lasts longer than 8 days.
- Bleeding occurs between periods.
- Regular occurrence of periods less than 21 days apart.
Changes in Mood
Some can experience mood swings, irritability, or depression during perimenopause, one minute you’re a zen goddess, the next, you’re rage-texting your group chat because someone forgot to replace the toilet paper roll (again). So, what’s the deal with these mood swings, irritability, and bouts of the blues?
Well, here’s where the science gets a little murky. Some experts blame shifting estrogen levels, claiming that your brain is basically being punked by your hormones. Depression? Anxiety? Irritability? All allegedly courtesy of that estrogen exodus.
Your body is throwing a hormonal tantrum and you’re dealing with the physical side effects of menopause, which—spoiler alert—can be pretty mood-wrecking on their own. Basically, perimenopause is like the ultimate bad roommate: messy, unpredictable, and always interrupting your sleep.
Perimenopause & Menopause Can Cause Anxiety and Panic Attacks
Let’s be real: as if the random hot flashes, sleepless nights, and forgetting why you walked into a room weren’t enough, there’s another fun sidekick that often joins the party—anxiety. Yep, anxiety and panic attacks love to pop up uninvited during this phase of life, like the worst kind of surprise guest who eats all the snacks and clogs your emotional sink.
If you’ve already dealt with anxiety in your life (because being a woman in this world isn’t stressful enough), menopause can take that familiar tension and turn it up to 11. For some, it even escalates to full-blown panic disorder, like your brain decided to add fireworks to an already intense bonfire. Studies show women between 50 and 79 are prime targets for panic attacks. What’s that about, nature? Thanks a lot.
So, what does a panic attack feel like? Glad you asked (but also sorry, because ugh). Panic attack symptoms can mess with both your body and your brain, leaving you wondering if you’re losing it. Here’s a rundown of what might happen when anxiety decides to crash your menopause party:
- Heart palpitations
- Chest pains
- Sweating
- Shaking
- Nausea
- Dizziness
- Sense of doom
- Numbness
- Anxiety
- Chills
When it comes to tackling menopause-related anxiety, it’s time to bring out the big guns—and by "big guns," I mean whatever works for you because this stage of life isn’t one-size-fits-all. First up, there’s low-dose hormone replacement therapy (HRT), the Beyoncé of menopause treatments—powerful and effective when used the right way.
If HRT isn’t your jam, don’t sweat it. Antidepressants and anti-anxiety meds can be lifesavers, while good old-fashioned therapy (yes, talking about your feelings does help) is always a solid option. Then there’s the “eat your veggies” pep talk: A nutrition-focused diet is like a hug for your brain chemistry, and mood-boosting supplements can also work wonders.
Oh, and about sugar? It might feel like your BFF during a tough day, but trust me, it’s a shady friend who stabs you in the back with extra anxiety later. Keep the chocolate cake as an occasional fling, not a full-blown relationship.
Why Talk Therapy and CBT Alone Might Not Cut It for Menopause
Listen up, ladies—this is not just in your head. Nope, it’s in your hormones, and they’re throwing a full-on rave without your permission. This is a real, physical thing, not something that a therapist can just chat away (and trust me, I am one, so I’d know).
As you navigate the grand finale of perimenopause and step into the VIP section of menopause, talk therapy isn’t going to cut it for those wild, hormone-fueled antics your body’s pulling. It’s time to focus on what’s really happening under the hood—not blame yourself for what’s entirely out of your control.
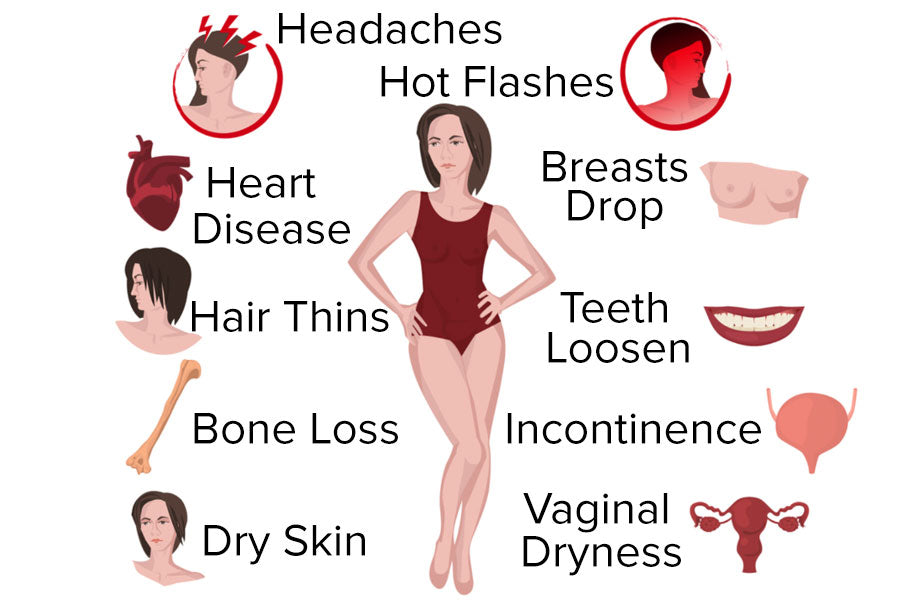
More Examples of Fun Things Can Happen?
- Lower Back Pain
- Joint pain: Knee Pain, Hip Pain (Bursitis), Joint Tenderness, Frozen shoulder
- Hot Flashes
- Brain Fog: Difficulty focusing
- Fatigue: Persistent lack of energy and motivation
- Difficulty Sleeping:
- Fluctuating rapid heart rate, especially noticeable at night, possibly causing dyspnea (shortness of breath)
- Estrogen dropping can cause a release of cortisol, adrenal and lowering serotonin levels for what can feel like high levels of anxiety
- Low Sex Drive: Not psychological in nature
- Dry Eyes: Impairs vision and may resemble an astigmatism at night
- Dry Skin
- Dry Mouth
- Dry Sinuses: Can lead to sinus headaches
- Vaginal Dryness
Estrogen Patches: A Really Great Option
First up, estrogen patches—they’re like the chill, low-risk cousin of oral estrogen. Less risky, easier on your system, and if you’re not already taking progesterone orally, you can go for a combo: estradiol patch with micronized progesterone.
Estrogen patches are like the VIP pass for your hormones—they skip the liver, go straight into your bloodstream, and avoid the drama. Oral estrogen, on the other hand, has to detour through your digestive system and liver, which can stir up trouble like blood clots and gallbladder issues.
Plus, patches keep your hormone levels steady (no wild rollercoasters), and they’re a lot gentler on your heart. So, think of patches as the chill, low-risk option for hormone therapy.
Typically, doctors suggest estrogen therapy for about 10 years, but it all depends on your health and needs. So yes, this one’s worth bringing up with your healthcare provider.
Pro Tip: Keep Your Estrogen Patch In Place
Estrogen patches have to stay on for a seven-day work week and having them come off can sometimes be a struggle. Let’s be real, hot showers, baths, and life in general can turn them into escape artists.
The fix? Steal a page from the tattoo crowd’s playbook and slap a Tattoo Aftercare Bandage over your patch. It’s like a tiny raincoat for your hormone hero—keeping it secure, dry, and ready to crush its weeklong to-do list.
Nervous About Risks? Read This Study
If you’re worried about hormone therapy risks, take a deep breath and read this study from the American Heart Association. It’s chef’s kiss for explaining how hormone therapy—when started before age 60 or within 10 years of menopause—can actually reduce risks for:
- Cardiovascular disease
- All-cause mortality (aka dying for any reason)
- Certain cancers
The study is crystal clear, and I highly recommend printing it out and taking it to your next doctor’s appointment if you’re considering hormone therapy. It’s always nice to have some solid science on your side.
Why Oral Progesterone Might Be the Better Choice for You
Let’s talk about progesterone. It’s one of those hormones that doesn’t get as much attention as, say, estrogen, but it’s a VIP when it comes to managing hormonal health. If you’re weighing your options between oral progesterone and a patch (or cream, or gel), here’s the scoop on why the pill might just be the MVP of hormone therapy.
First up, oral progesterone is like that friend who always shows up on time and never cancels plans. It’s reliable. When you take it, you can count on consistent levels of progesterone in your body, which is a big deal for keeping things running smoothly. This is especially important if you’re also on estrogen therapy. Oral progesterone protects the lining of your uterus like a bouncer at an exclusive club, making sure it doesn’t get too crowded or unruly (a.k.a. preventing endometrial issues).
But wait, it gets better. Oral progesterone has a little secret superpower: it helps you sleep. If you’re lying awake at night counting sheep, oral progesterone’s calming effect can be a total game-changer. It produces something called allopregnanolone, which sounds fancy but basically translates to "sleepy magic." So, if menopause has turned your nighttime routine into an insomniac's Olympics, this could be your ticket back to dreamland.
And let’s not forget about the ease of popping a pill. No sticky mess, no waiting for things to dry, no weird smells that make your dog suddenly very interested in your ankles. It’s quick, it’s painless, and it just works.
Of course, there’s always a time and place for a patch or a cream. Maybe oral progesterone makes you feel too drowsy, or your doctor thinks your liver deserves a break. Or maybe you just really enjoy the ritual of slathering things on your skin. Totally valid.
The best choice for you depends on your body, your life, and how much patience you have for waiting around with a patch glued to your thigh. Talk to your doctor, listen to your body, and don’t be afraid to try different options until you find what makes you feel like your best self.
Vaginal Estrogen Cream: A Big Win
If you’re not already using vaginal estrogen cream, I’m here to tell you, you’re missing out. This magical stuff isn’t systemic (meaning, no scary risks) and works purely on a topical level. But wait, it gets better.
For Sexual Health: Using this in the vagina is standard, but put a dab on your clitoris as it makes your body way more responsive during sex. Translation: easier orgasms and less time waiting for your body to get with the program. (Who doesn’t want that?) You use it vaginally 3 days a week, so it is not even needed every day.
For Your Skin: Slather it on your face, hands, or wherever you want a little youth boost. Many users, including yours truly, have noticed firmer, more youthful-looking skin after just a few months of use. I use it on my face daily, and you can keep using this cream forever—no time limit here. Seriously, vaginal estrogen cream deserves a standing ovation.
Telehealth Companies That Prescribe and Ship Estradiol Patches & More
-
Evernow: Specializes in hormone replacement therapy (HRT) for menopause, including estradiol patches. They prescribe via online consultations and ship nationwide.
-
PlushCare: Offers HRT prescriptions and partners with pharmacies to deliver medications, including estradiol patches, across state lines.
-
Hers (for Women): Provides hormone therapy for menopause and ships prescriptions to most states.
-
Midi Health: Focuses on menopause care, offering personalized treatment plans and shipping medications like estradiol patches nationwide.
- Alloy Health: Prescribes and ships FDA-approved HRT options, including estradiol patches, directly to patients.
Herbal Supplements
Herbal supplements that can help calm the body are holy basil (tulsi), chamomile, hops, passion flower, ashwagandha, lemon balm, kava, and others. Make sure to check with your physician or pharmacist regarding any herbs you take, as they too are a form of drugs and may affect other health conditions or interfere with medications you may be taking.
Anxiety & Related Cardiovascular Symptoms
Hormonal fluctuations during menopause may negatively affect the cardiovascular system. Perimenopause and menopause may cause heart palpitations. First, it is essential to rule out heart conditions by working with your physician, especially a cardiologist, because post-menopausal women are more likely to develop heart disease and arrhythmia than pre-menopausal women.
It is typical for cardiac arrhythmias such as an abnormally fast heart rate, leading to shortness of breath, chest pain, and severe anxiety. Women who experience fast heart rates (tachycardia) may be prescribed medications known as beta-blockers, which can regulate the heart's rate and rhythm and ease other physical manifestations of anxiety, including sweating, shaking, hyperventilation, and apprehension.
How To Redirect Your Brain When You Feel Panic & Anxiety
- Stay focused on the present and ask yourself what you can do when experiencing worry. If you are safe and alright, make a time where you will check in with yourself to revisit your concerns when you are in a better emotional place.
- Relabel your feelings when you feel panic. Often, it can feel like you are dying or having a heart attack. Remind yourself that this is a panic attack and tell yourself that it is temporary and that you do not need to do anything right now.
Your body is activating its flight or flight response to keep you alive, and it is essential to refocus your mind to understand that you are safe and alright. If you can, crying is an excellent way to release these challenging feelings as it activates the vagus nerve and parasympathetic system. It can relieve stress and decrease cortisol levels in the body.
- Fact check your thoughts by challenging how realistic they are, so instead of focusing on feeling anxious, say things to yourself that assure yourself that you are alright, prepared and that things will go well. Rethinking your fears trains your brain to deal with your anxious thoughts.
- Breathe in and out slowly by evenly inhaling and exhaling. This will help slow down and refocus your mind.
- Follow the 3-3-3 rule by naming three things you see and hear. Then move three parts of your body (i.e., touch a finger to your nose, lift a leg and pat your head three times). By doing this, you are activating a different part of your brain, which will help manage your emotions.
- Do a task such as get up and put something away, get a glass of water or action as it will interrupt your anxious train of thoughts and help you feel more in control.
- Stand up straight and pull your shoulders back with your feet apart. When we are stressed, we hunch, and it makes us feel as though we are cowering to protect ourselves. When we stand up straight, we can feel more in control.
- Process your feelings with a trusted friend or partner and ask them how realistic you are about your worries. You can also write out your fears to better see what you are worrying about.
- Watch something funny, especially short clips that quickly redirect your attention. Laughing allows us to release tension and lowers anxiety.
- Exercise to release pent-up energy and channel it into a physical activity that makes you sweat. This helps the body boost your endorphins which make you feel good.
- Use paired muscle relaxation to relieve tension. While taking a deep breath in, tense the muscles of your entire body. Notice how that tension feels. When you breathe out, let go of all that tension and notice the changes you feel in your body. You can also try tensing specific muscle groups such as legs, arms, etc.
- Sit or take a walk outside in nature or simply watch the clouds pass. Nature is known to improve mood, reduce anxiety, lower blood pressure and stress hormone levels, reduce nervous system arousal, enhance immune system function, and increase self-esteem.
- Redirect your stress by giving your body something to taste. For example, drinking relaxing herbal tea, chewing gum, or sucking on sugar-free candy can help you to relax.
- Using scents to lift your mood can be helpful. Using essential oils in diffusing oils, wax melts, or scented candles can be beneficial. Even putting on your favorite scent can help you to relax.
- Massage, acupuncture, relaxing baths, and other forms of physical soothing can allow you to destress.
- Listening to your favorite music, using a sound machine, and repeating positive affirmations can help reduce stress.
Reset The Vagus Nerve During Anxiety: Polyvagal Theory Exercises
Resetting the vagus nerve, which interfaces between the central nervous system and consists of the brain and the spinal cord, can be helpful as it can release anxiety that is physiologically happening in the body. You can do this through polyvagal exercises. Examples of this:
- Hold your face under cold water for 15 to 30 seconds or put a ziplock bag over your face with ice water in it. This will trigger your brain to think it is diving underwater, slowing your heart rate.
- Using vocal sound can help stimulate the vagus nerve as it is located near the vocal cords. To do this, yoga practitioners recommend the "om" chant or other mantras, but simply humming any song can have the same effect.
- Lie on your back, interlace your fingers, and place them behind your head at the base of the skull. Keeping your head straight, move your eyes to the right, sigh, swallow or yawn and then move your eyes to the left and do the same; you may blink during the exercise. Do this for about five minutes or until you feel calmer.
Paresthesia
Paresthesia is an abnormal sensation of the skin (tingling, pricking, chilling, burning, numbness, itching) that can occur due to a sharp decline in estrogen. It can cause distress in women who experience it. Vitamins and minerals such as biotin, magnesium, vitamin C, and omega-3 fatty acids may assist with skin issues during menopause.
Sleep Disturbances
Those who have slept soundly their entire lives may find that fluctuating hormone levels wreak havoc with their sleep cycle. Hot flashes or night sweats often cause difficulties falling asleep or staying asleep along with hormonal fluctuations.
Hot Flashes
It is essential to stay hydrated because hot flashes and night sweats cause profuse sweating; they can also cause electrolyte loss through perspiration, dehydration, and insomnia.
Itchy Skin
Itchy skin is something that is often overlooked when it comes to menopause. However, some women may experience itchy skin (pruritus) all over their bodies, including itchy sensations inside the ears. An itch inside ears, which can be intense, is often misdiagnosed by physicians as eczema or other ailments when in reality, it is just part of perimenopause or menopause. However, keep in mind that hormone levels that change during menopause can lead to some women developing eczema.
Vaginal Changes and Bladder Problems
Estrogen plays a crucial role in maintaining the function of the vagina and surrounding tissues, uterus, urinary bladder, and urethra (the organ through which urine is passed from the bladder). As these tissues weaken, they can lead to the involuntary leakage of urine, infection, or painful urination. The vaginal tissues also become less lubricated, which can cause uncomfortable or even painful sexual intercourse and more frequent urinary tract infections.
See our Kegel Exercise Guide and Kegel Weights Guide to prevent or help with urinary incontinence.
Decreasing Fertility
As hormones fluctuate and ovulation becomes irregular, your ability to conceive decreases. As long as you have periods, pregnancy is a possibility. If you do not want to conceive, it is recommended that you use birth control until you have reached menopause and have not had a period for 12 months.
Bone Loss
As estrogen levels decline, you naturally begin to lose bone more quickly than you replace it, thus increasing your risk of osteoporosis. The best things that you can do for your bones are below:
- Get enough calcium and vitamin D3 and eat a well-balanced diet. Plant-based is ideal as fruits and vegetables are nutrient-dense and high in fiber, which helps regulate hormones.
- Avoid smoking and limit alcohol. See our article on Wine, Chocolate & Health Guide for more information.
- Engage in regular exercise like walking, yoga, cycling, etc. If you have osteoporosis, avoid high-impact exercises or activities in which a fall is likely. Also, avoid activities that put weight or heavy stress on the spine to prevent fractures.


Change in Cholesterol Levels
Declining estrogen levels may also negatively affect your blood cholesterol levels. This could include an increase in low-density lipoprotein (LDL) cholesterol (the "bad" cholesterol), which contributes to an increased risk of heart disease. At the same time, high-density lipoprotein (HDL) cholesterol (the "good" cholesterol) decreases in many as they age, which also increases the risk of heart disease.
Low Libido
You may find your sexual desire and arousal change during perimenopause. Hormonal imbalance is the most common cause of low sex drive during this phase of life. The hormone progesterone plays a significant role in libido. As progesterone levels drop, it can affect your sexual desires and state of arousal.
However, keep in mind that libido may not decline with the onset of menopause because estrogen declines more than testosterone. Thus, some theorize that a lower sex drive should not be an issue because of estrogen reduction. The decline in testosterone is related to age, not menopause, and begins years before perimenopause.
Declining estrogen levels also affect testosterone, which plays a role in sexual response and orgasm. Fatigue caused by hormonal imbalance and poor nutrition can also affect your interest in sex.
Sexual Aids For Perimenopause & Menopause
The symptoms of perimenopause result from changing hormone levels that some begin noticing long before menopause takes place. Using sexual aids such as sex toys, lubricants, Kegel exercisers, and even dilators can be helpful.
Vibrators
Vibrators help increase blood flow to the genital area and thus bring helpful circulation, which can aid in increasing the sex drive (libido), increase lubrication, and assist in achieving orgasms. See our guide on How To Choose A Vibrator.
Lubricants
Lubricants help reduce friction during vaginal penetration and be used as vaginal moisturizers to help with vaginal dryness that can cause painful sex during perimenopause and menopause. See our helpful Lubricant Guide for helpful tips.
Dilators
Sometimes during perimenopause or menopause, vaginal tissue can become dry, making sex painful. With sexual inactivity, the vaginal walls may also become tight, making sexual penetration more difficult. Using dilators to stretch can be helpful.
Kegel Weights
Kegel weights and exercisers can help make the vagina feel tighter and more snug which can improve one's sex life. However, the most common reason is that many struggle with urinary incontinence, causing embarrassing leaks, especially when laughing, sneezing, coughing. This can be exacerbated by childbirth recovery, weak pelvic floor muscles, and pelvic organ prolapse. Doing Kegel exercises with or without Kegel weights for just 10-15 minutes a day can make a big difference.
Lifestyle Modifications
Exercise
Recommendations are three to five days a week of exercise, including resistance or weight training with weights, bands, machines, and cardiovascular activity such as brisk walking, cycling, swimming, or aerobic type classes. Also, stretching should be done most days of the week to maintain range of motion. Yoga, pilates, and tai chi classes can be a valuable activity of this age group.
Why Is Exercise So Important?
- Engage in regular exercise as it increases the cardiorespiratory functioning and reduces metabolic risks associated with declining estrogen.
- Exercise increases HDL, reduces LDL, triglycerides, and fibrinogen, which lowers the risk of high blood pressure, heart attacks, and strokes.
- Exercise minimizes midlife weight gain. It increases the metabolism to burn off the extra fat gains associated with hormones change. Also, see our Weight Loss Guide.
- Exercise also increases bone mass and can help offset the decrease of bone mineral density and prevent osteoporosis.
- Reduces lower back pain associated with perimenopause and menopause. Research has associated low estrogen levels with more severe lumbar disc degeneration and increased lower back pain in menopausal women.
- Exercise reduces stress and improves mood. Exercise releases endorphins in the brain, which stimulates a feeling of well being that can last several hours and help alleviate some depression and mood swings.
- It may reduce hot flashes, and studies have shown that hot flashes are also less common among physically active people who exercise regularly.
Nutrition
As your risk of heart disease and osteoporosis increases at this time, a healthy diet is more important than ever. Choose a low in saturated and trans fats and high-fiber diet that's rich in fruits, vegetables, beans, and whole grains such as steel-cut oats. Add calcium-rich foods or take a calcium supplement if your physician suggests it. Eat things like dark leafy greens, which are a great source of calcium, which is essential for maintaining bone health.
The Controversy Of Phytoestrogens In Soy
Soy products contain important isoflavones, and it has been proven that soy products are associated with fewer hot flashes. We recommend soy products high in isoflavones: green soybeans, soy flour (textured), dry roasted soybeans, tempeh, soybean curd cheese, tofu, tofu yogurt, soymilk.
Soy comes from soybeans and is consumed in various ways, such as eating them steamed (edamame), tempeh (fermented soybeans), and soy flour and milk. Soy has high amounts of phytoestrogens, so there has been controversy around its effects on sexuality. There have even been false claims that they increase estrogen levels and increase breast cancer risks. Let's explore why that is not correct.
Your body knows the difference between estrogen and plant-based phytoestrogens. We know this because of the receptors that are used to process them. There are two estrogen receptors in the body, alpha (A receptor) and beta (B receptor). Unlike actual estrogen, which binds to A receptors, soy phytoestrogens bind to the B receptors. This is critical because each receptor has completely different ways of distributing the estrogen and phytoestrogen hormones.
A medical study done in 2004 shows that because the B receptors distribute phytoestrogens, they have an anti-estrogenic effect, meaning that it inhibits actual estrogen. This means that eating phytoestrogens in soy products will not increase estrogen levels.
Websites scaring people away from eating soy, claiming that it contributes to estrogen-related cancers, are wrong, and many studies support that this is false. This also means that those holistic websites promoting it to increase estrogen in perimenopausal and menopausal women are also incorrect.
So how did this rumor that soy causes an increase in estrogen occur? It was based on a study that tested breast cancer in mice, but it turns out that we metabolize soy isoflavones very differently from rodents. Not only that, it turns out through multiple studies that soy actually reduces our chances of breast cancer if eaten regularly. This was further validated and published in 2009 in the Journal of the American Medical Association. It is also why the American Cancer Society recommends consuming soy.
We highly recommend nutrition based on the books "How Not To Die," By Michael Greger, M.D. FACLM and "Eat To Live" by Joel Fuhrman, M.D.
For more information, see our Nutrition Guide for Good Sex & Health Guide.
Reduce or Eliminate Stimulants
I am sure that this isn’t your first rodeo hearing that smoking, boozing, and caffeine-chugging aren’t exactly the holy trinity of health. But here’s the tea (decaf, preferably): if you’re in the throes of perimenopause or menopause, it’s time to rethink your vices—because these habits can mess with you in ways even your moody hormones wouldn’t dare.
Smoking? It’s not just bad news for your lungs and heart; it’s like kryptonite for your bones. We’re talking weaker, brittle bones that are basically the equivalent of trying to use a soggy pool noodle for self-defense. Nobody wants that.
As for alcohol, let’s just say moderation is the new party. Experts suggest capping it at one drink a day (sorry, not per hour). Why? Beyond the hangovers from hell, alcohol can weaken your bones and has been linked to a higher risk of breast cancer. So, maybe skip that second glass of rosé and save it for when your favorite show drops a new season.
And caffeine? That sweet, jittery nectar of life? It’s the ultimate two-faced frenemy. Sure, it keeps you awake for your kid’s third retelling of The Lorax, but it’s also the sneaky culprit behind hot flashes that make you feel like you’re auditioning for Survivor: Sahara Edition. Plus, it can totally wreck your already fragile relationship with sleep.
So, what’s the takeaway? Cut back on the stuff that makes your body feel like it’s rebelling against you. Because, girl, you deserve to feel fabulous—even when your hormones have other plans.
Stress Reduction
Stress and perimenopause go together like toddlers and sharpie markers—messy, chaotic, and almost impossible to clean up. That extra dose of stress we carry around? It’s not just annoying; it throws our bodies, minds, and spirits completely out of whack and turns perimenopause into a whole circus of symptoms. Cue the clown car of hot flashes, mood swings, and sleepless nights.
But here’s the good news: you don’t have to sit there juggling flaming stress balls. Stress-busting techniques like meditation, yoga, and even some good ol’ self-imagery (that’s a fancy way of saying "daydreaming about being on a beach with zero Wi-Fi") can be total game-changers. They’re like pressing pause on the chaos and letting your body take a breather.
Now, I know what you’re thinking: When exactly am I supposed to find time to meditate? Between managing work, and trying not to scream at the slowest grocery store cashier in existence? Listen, I get it. Women are basically superheroes with terrible self-care habits. But here’s the deal: if you don’t make time to recharge, you’re running on fumes, and no one wins.
So go ahead—schedule some “me time” like it’s an appointment you absolutely can’t miss. Think of it as plugging yourself into a human-sized charging station. Whether it’s five minutes of stretching, ten minutes of mindfulness, or even a nap disguised as “deep meditation,” those little breaks aren’t indulgent—they’re essential.
Foot Massage
A study about how foot massage affects anxiety, fatigue, and sleep in postmenopausal women determined that foot massage applied during menopause can increase the average daily sleep duration and reduce fatigue and anxiety levels in women.
Postmenopausal women in the study reported catching more Z’s and feeling less wiped out—all thanks to a little TLC for their toes. And here’s the kicker (pun intended): this isn’t just some spa-day indulgence.
Regular foot massages—whether you rope in your partner, treat yourself to a pro, or even try some acupressure at home—could be a game-changer for your well-being. Menopause might still be throwing curveballs, but now you’ve got a secret weapon to step up your self-care game. So go ahead, put your feet first. They deserve it.
Complementary and Alternative Therapies
Complementary and alternative therapies are medical treatments that are considered nontraditional. They include dietary and herbal supplements, acupuncture, chiropractic and massage therapy, biofeedback, homeopathy, and eating certain foods that are thought to prevent disease or heal.
Alternative treatments are often used alone, while complimentary treatments are alternative treatments used in combination with traditional treatments, such as drug treatments or surgery.
Herbal remedies and supplements that have been shown to help counteract perimenopause symptoms while increasing overall health are listed below. Understand that herbs can be just as powerful as a drug and can interfere with medications, so make sure to review all of the herbs you take with your physician and research them thoroughly to ensure that they will meet your health needs and not cause health problems.
Bayberry (Morella Cerifera)
The fruit of the Bayberry tree can increase blood flow and capillary dilation in the mucus membranes of the vagina. This can increase vaginal lubrication. Bayberry also has beneficial effects on female reproductive muscle organs by increasing muscle tissue tone and circulation.
Black Cohosh (Cimicifuga racemosa, Actea racemosa)
A member of the buttercup family and native to North America. Some clinical research has shown that black cohosh is effective for the relief of hot flashes, night sweats, and vaginal dryness. This herb has been proven to reduce luteinizing hormone secretions. High levels of the luteinizing hormone are responsible for the onset of menopause.
Calcium
Essential for the normal growth and maintenance of bones and teeth. Perimenopause and menopause represent depletion of estrogen, which, in turn, is associated with increased risk of bone loss and heart disease. Should be taken with magnesium for optimal absorption.
Damiana (Turnera diffusa)
Damiana is a small shrub native to Mexico. The leaves are used for medicinal purposes. Damiana is considered a powerful aphrodisiac. It stimulates the sympathetic nerves' function controlling the sexual organs, the urinary system, the digestive organs, and the respiratory organs. The herb strengthens all the functions of the sexual organs and urinary system. This herb is especially effective. It has been shown to have the same effects as the hormone progesterone and regulating estrogen, which can benefit premenopausal and menopausal people.
Evening Primrose (Oenothera biennis)
A biennial herb common in North America Parts The seed oil is a good GLA source, an essential fatty acid. An essential fatty acid is a nutrient that the body can't make but is essential to good health. Evening Primrose Oil has been used for premenstrual syndrome ( PMS ) and mastalgia ( sore breasts ). Studies to date have been conflicting; some show a significant reduction in breast pain, while others fail to confirm this. There are no known contraindications or drug interactions reported.
Flax Seed Oil ( Linum Usitatissimum)
A perennial herb grows to 3 ft. with oily brown seeds, native to Europe and Asia. The seeds and seed oil contain essential fatty acids - palmitic, steric, oleic, linoleic, and linolenic. Flaxseed oil is a good source of essential fatty acids. Flaxseed oil is rich in (GLA) gamma Linolenic acid used by many for PMS and breast tenderness. No reports of toxicity when used at recommended doses.
Gingko Biloba
Many research studies have shown Ginkgo Biloba can assist in improving blood flow. Enhancing blood flow to the genitals heightens sexual sensations. Gingko Biloba significantly increases mental activity and memory. Since sexual desire begins in the brain, this herb can be a powerful sexual aid.
Ginseng (Panax quinquefolius)
The several Ginseng species are native to East Asia and Northern America. Ginseng stimulates neural functions and stimulates and normalizes cerebral and sexual organ blood flow. Ginseng also stimulates nerve growth, blood production, and sperm production. This stimulation will, in turn, give a revitalizing effect, stronger sexual arousal, improved genital function, and increased physical sensation.
Horny Goat Weed (Epidemium)
Epidemium is native to East Asia. The entire plant, except for the root, is used in herbal preparations. This herb stimulates the sexual organs, giving enhanced genital sensations. It can also increase sperm production, which may improve fertility. It further stimulates sexual desire by acting upon the central nervous system. This herb has been used for over 2,000 years as a libido enhancer for both men and women and improves erection in men.
L-arginine With Choline
This combination is recommended daily for promoting better blood flow to the pelvic organs and tissue to assist with low libido.
Maca (Lepidium Meyenii)
Maca is native to Peru and has been passed down as a legendary sex-enhancing root from the Incas. Maca root is known for it's the ability to stimulate sexual desire and drive, increase energy, libido, and sexual function. This Peruvian herb may also help with hot flashes and night sweats.
Magnesium
Helps with calcium absorption, acts as a muscle relaxant, produces a sense of calmness, reduces mood swings and irritability, promotes a peaceful night's sleep, and reduces food cravings.
Natural Progesterone Cream
Natural progesterone creams usually contain extracts from Mexican wild yam, a substance that is believed to be similar to the body's progesterone. Many have found natural progesterone creams to be very effective in treating menopause symptoms. Still, there is no evidence to show that the creams lower the risk of breast and uterine cancer, or are free from side effects as is sometimes claimed.
Peppermint (Mentha Piperita)
Leaves of the peppermint plant stimulate genital secretions, which enhance lubrication. This facilitates the sexual act and protects the sexual organ against injury.
Sage (Salvia Officinalis)
The leaf of the sage plant has been used medicinally for centuries. Sage leaf will assist in improving mental focus energy restoration. Sage is a natural antiperspirant that contains estrogen-like substances to help alleviate "hot flashes" and the adverse reactions to hormonal changes.
Suma (Pfaffia Paniculata)
Suma is native to the Amazon Basin. The indigenous people of the Amazon have been using Suma for centuries as a sexual tonic. Suma root is an adaptogen that normalizes hormone production, increases libido, and calms nerves. An improved hormonal system can, in turn, improve mental and physical sexual function.
Valerian (Valeriana Officinalis)
Sleep disturbances are common during perimenopause caused by hormonal fluctuations. Valerian is an effective herbal supplement that decreases the time it takes to fall asleep, improves sleep quality, and reduces the number of night awakenings, all without any associated daytime drowsiness.
Vitamin B6 (Pyridoxine)
Natural sources of vitamin B6 are whole grains, bananas, potatoes, nuts and seeds, and cauliflower. Vitamin B6 levels can be helpful in those who are deficient and suffering from depression. Pyridoxine, folic acid, and vitamin B6 deficiencies have also been associated with osteoporosis in postmenopausal people. At least ten studies have been done on pyridoxine use for PMS and improved PMS symptoms with pyridoxine supplementation. Vitamin B6 is also associated with a decrease in the incidence of heart disease in women. Vitamin B6 is safe when taken in recommended dosages.
Vitamin C
Best when taken with Bioflavonoids (such as Hesperidin), helps boost the immune system, reduce hot flashes, and aid the adrenal glands.
Vitamin E (d-alpha-tocopherol)
An antioxidant found in high amounts in polyunsaturated vegetable oils, wheat germ, seeds, and nuts. In natural vitamin E, the small d in d-alpha-tocopherol signifies a natural source preferable to synthetic vitamin E signified by the dl in dl-alpha-tocopherol. Mixed tocopherols contain d-alpha, beta, delta, and gamma tocopherols. Mixed tocopherols offer the most significant benefit. Look for natural mixed tocopherols. Vitamin E has been shown to help in reducing hot flashes and vaginal dryness. Vitamin E potentiates (cause a more significant effect) of anticoagulant drugs such as Coumadin or aspirin. If you are on either of these drugs, consult your doctor or naturopath before starting vitamin E.
Traditional Medical Treatments
If you have severe symptoms, you may want to ask your doctor about prescription medicines. Some choices include:
Low-dose hormone replacement therapy (HRT)
Think of HRT as the body's way of getting a hormone top-up when your ovaries decide to clock out. It's like giving your system a little nudge to help manage those delightful symptoms like hot flashes, night sweats, and mood swings.
Back in 2002, the Women's Health Initiative (WHI) study threw some serious shade at HRT, suggesting it might do more harm than good. Cue the mass exodus of women ditching their prescriptions faster than you can say "hot flash." But hold up—turns out, the study's findings were a bit like a bad game of telephone: misinterpreted and blown out of proportion.
Fast forward to today, and the North American Menopause Society (NAMS) has given HRT a much-needed glow-up. For healthy women under 60, and within 10 years of menopause onset, the benefits of HRT often outweigh the risks. It's like the comeback tour we didn't know we needed.
While HRT isn't the fountain of youth, it's pretty darn effective at easing menopausal symptoms. But remember, it's not a one-size-fits-all solution. Your health history, symptoms, and personal vibes all play a role in deciding if HRT is your new best friend. So, grab a cup of tea (or wine—we don't judge) and have a heart-to-heart with your healthcare provider.
Menopause isn't a one-woman show; it's a shared experience with a variety of supporting acts. Whether it's HRT, lifestyle tweaks, or other treatments, you've got options. Stay informed, stay fabulous, and remember: menopause may be inevitable, but suffering through it is not.
Perimenopause & Menopause Empowerment
Before you decide on a game plan, take a moment to revisit your medical history and personal beliefs. Are you a fan of natural remedies, or do you prefer the reliability of modern medicine? Knowing where you stand will help you set clear goals for managing your symptoms.
Option 1: Lifestyle Changes
If you're leaning towards a natural approach, consider embracing lifestyle modifications. An anti-inflammatory diet, like the one advocated by Dr. Mary Claire Haver in The Galveston Diet, focuses on healthy fats, lean meats, a variety of fruits and vegetables, and whole grains.
Regular exercise, stress reduction techniques, and quality sleep are also key players in this strategy.
Option 2: Herbal Remedies and Acupuncture
For those who trust in the wisdom of ancient practices, herbal supplements and acupuncture might be appealing. However, it's important to note that, as of 2023, there is no consistent evidence supporting the efficacy of acupuncture in managing menopausal symptoms.
Always consult with a healthcare provider before starting any new treatment to ensure it's safe and suitable for you.
Option 3: Medication
If you're open to medical interventions, Hormone Replacement Therapy (HRT) is a viable option. Recent studies have shown that HRT can effectively alleviate symptoms like hot flashes and mood swings, especially when started within ten years of menopause onset.
Discuss with your doctor to determine if this is the right path for you, and if you doctor does not agree with you, get a second opinion! You are the one in charge of your health. See our article How To Talk To Your Doctor About Sex for more tips.
The Non-Negotiables: Diet, Exercise, Stress Reduction, and Sleep
Regardless of the path you choose, some fundamentals remain essential:
Eat a Healthy Diet:
Incorporate anti-inflammatory foods to help manage symptoms and promote overall health.
Exercise Regularly:
Engage in both resistance training and aerobic activities to maintain muscle mass, bone density, and cardiovascular health.
Reduce Stress Levels:
Techniques like mindfulness, meditation, and breathing exercises can help manage stress.
Get Enough Sleep:
Aim for 7-8 hours of quality sleep each night to support overall well-being.
Remember, this is your journey, and you have the power to choose the path that aligns with your values and lifestyle. Embrace the change, take care of yourself, and know that you're worth every bit of effort you invest in your health.
A Good Resource
If you want to go down another great menopause education rabbit hole, let me introduce you to Dr. Mary Claire Haver. She’s a colleague of mine and an OBGYN with no-nonsense advice and science-backed tips. She’s the one who first turned me on to the study about how estrogen patches are less risky than oral estrogen.
She’s also got a website, The Pause Life, and her calcium and other supplements are spot-on for what you need—unlike some of the stuff you’ll find at other places.
See more of our helpful menopause resources as well:
Menopause Brain: It's Real, Let's Talk About What You Can Do About It
HRT & Strength Building: Why Women Need to Rethink Aging